How do I test for pre-diabetes?
Medical review by
Dr Alasdair Scott MBBS FRCS PhDLast updated
Key Article Takeaways
- Having “pre-diabetes” means that your body is struggling to control your blood sugar and you’re at high risk of getting diabetes.
- Pre-diabetes is a “warning-shot” - it’s reversible and you can avoid diabetes but you need to act now.
- You won’t have any symptoms with pre-diabetes so the only way to know is to test.
- Take our Pre-diabetes and Sugar Handling HbA1c Test to find out if you’re pre-diabetic.
You’ve almost certainly heard of diabetes, but what about “pre-diabetes”? Pre-diabetes is important and we’re here to explain why. We’ll also cover how to test for pre-diabetes, what your results mean and how you can act now to prevent diabetes and stay on top of your health.
What is diabetes?
Diabetes is where your body has trouble controlling the level of glucose (sugar) in your blood. Your body keeps your glucose levels tightly controlled. If levels are too low, you don’t have enough energy. Too high, and the glucose causes damage to blood vessels and organs1.
One of the key ways your body controls glucose levels is with the hormone insulin. Insulin pushes glucose into your cells, lowering your blood sugar level. This is exactly what happens when you eat. You absorb sugars from your food, which increases blood glucose levels. In response, your body releases insulin to drive the glucose level back down and keep blood sugar levels in balance.
Diabetes comes in two flavours - type 1 and type 2. Type 1 diabetes usually starts in childhood and is caused by damage to the cells which produce insulin. We’re not 100% sure what causes this damage though. Type 2 diabetes usually affects adults and, although you do make insulin, your body can’t respond to it well enough to keep your glucose levels in balance.
In this article we’ll focus on type 2 diabetes. In the UK, 9 in 10 people with diabetes have type 2 diabetes2.
Type 2 diabetes is generally caused by your lifestyle and diet along with genetics and family history. If you’ve got a parent or sibling with type 2 diabetes, you’re two to six times as likely to develop the condition. Also, certain populations like South Asian, African-Caribbean or Black African are at higher risk than others3.
What is pre-diabetes?
Pre-diabetes, sometimes called borderline diabetes, is when your body starts to show signs of not controlling blood sugar as well as it should. You won’t have any symptoms with pre-diabetes and your blood sugar levels can be normal or near to normal.
Pre-diabetes is a “warning-shot” for diabetes. Type 2 diabetes isn’t a sudden thing that happens overnight. It develops over time. You go from normal sugar control to pre-diabetes to diabetes, as shown in figure 1.
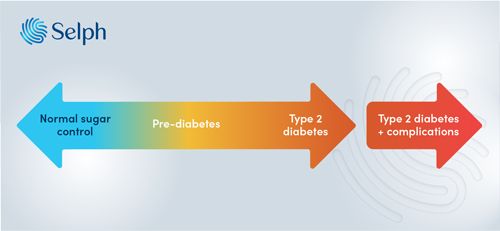
Figure 1. Sliding scale from normal sugar control to type 2 diabetes. Losing your ability to control blood sugar levels moves you along the scale from left to right. You can improve your blood sugar control to move from right to left. You can go in both directions until diabetes progresses too far. Once you start getting diabetes with complications you can’t go back.
Why is pre-diabetes important?
In pre-diabetes your body is starting to show signs that it’s unable to control your blood sugar levels, and you’re at high risk of progressing to diabetes. Every year, 5-10% of people with pre-diabetes will go on to develop full-blown diabetes4. Getting diabetes involves taking medication for the rest of your life and comes with lots of health complications.
Your body can cope with a poor diet, too much alcohol and a lack of exercise up to a point. Pre-diabetes is the sign that you've reached that point and your body can't cope any more. Pre-diabetes is also associated with increased risk of other conditions such as heart disease, stroke, cancer, dementia and joint problems to name a few5, 6, 7.
Crucially, pre-diabetes is reversible. Getting back normal glucose control even for a short time can lower your chance of getting diabetes by 50-70%8.
You can avoid getting diabetes, but you need to act now. We’ll give you some tips on how to do this. But first, how likely are you to be pre-diabetic?
Who's likely to get pre-diabetes?
Pre-diabetes is very common in the UK and more and more people are getting it. Right now it affects more than 1 in 3 adults and this is expected to rise even further9.
There are proven “risk-factors” for getting pre-diabetes and also diabetes. We’ve summarised these in table 1 below. Risk-factors like weight are modifiable. You can impact them by making changes, like through diet or exercise. Other risk-factors are non-modifiable. These are things you can’t change, like your age or if you’ve got relatives with diabetes.
| Modifiable risk-factors | Non-modifiable risk-factors |
| Weight | Age |
| Waist measurement | Sex (men are at higher risk) |
| Amount of physical activity | Family history of diabetes |
| Diet | Ethnicity |
| Alcohol consumption | Medical history of high blood pressure |
| Psychological stress | |
| Amount of sleep |

There are some quizzes for calculating your risk of getting type 2 diabetes. If you have a moderate to high risk but no symptoms, you could be pre-diabetic.
With no symptoms, the only way to find out if you’ve got pre-diabetes is to do a test.
How do you test for pre-diabetes?
How can you know if you’re pre-diabetic without any symptoms? There are handy tests we can do to find out if your body is not keeping your blood sugar levels in balance.
The main way we can tell if you have pre-diabetes is by doing a blood test for something called HbA1c. Sugar in your blood sticks to some of the haemoglobin in your red blood cells. Higher blood sugar means you have more glucose stuck to haemoglobin. This sugary haemoglobin is called HbA1c. How much HbA1c you have can tell us your average blood sugar levels in the last 2-3 months10. If you’re pre-diabetic then you’ll have higher than normal HbA1c levels, but below diabetic levels.
You can take our quick and easy Pre-diabetes and Sugar Handling HbA1c Test to find out if you’ve got pre-diabetes or diabetes itself. This is an easy finger-prick blood test which you can do at home and post back to our lab.
If you're over age 40, we recommend doing a general health screen once or twice a year. Think of it like getting your car MOT'd. Our broadest blood test panel is our General Health Blood Test. This checks your HbA1c, cholesterol and a host of other biomarkers including vitamins, kidney function and liver function. Alternatively, we also offer a more focused Cholesterol and Heart Health Blood Test which includes HbA1c and cholesterol.
Another way to diagnose pre-diabetes is by taking what's known as an "oral glucose tolerance test" or OGTT for short11. An OGTT involves drinking a sugary glucose drink and then taking blood measurements at intervals to see how well your body controls your sugar levels. You can do this with your GP.
What does my HbA1c level mean?
Table 2 below shows different HbA1c levels and the diagnosis you would get for each.
| HbA1c (mmol/mol) | Diagnosis |
| 30 - 35 | Optimal |
| 35 - 39 | Normal |
| 39 - 47 | Pre-diabetes |
| 48 and above | Diabetes |
Does a normal HbA1c level mean you’re in the clear? Sadly not. Having a normal HbA1c level doesn’t mean that you won’t ever get diabetes. HbA1c should be something you monitor regularly because you can see your own unique trend. Your HbA1c could be climbing little by little each time you test it. This can signal that you need to make some lifestyle changes to stabilise or lower it before it gets into the pre-diabetes range.
Being in the pre-diabetic HbA1c range doesn’t mean you’ll definitely get type 2 diabetes. Your body is showing signs of not handling glucose as well as it should and it does mean that you’re more likely to get diabetes if you don’t make any changes. But you’re not there yet and you still have the opportunity to turn things around.
Whatever your starting HbA1c, you can test yourself regularly to keep track of your levels and steer the course of your own health.

So, I’m pre-diabetic - what should I do?
The main way to prevent diabetes and reverse pre-diabetes is by increasing exercise levels and prioritising a healthy diet. These are lifestyle changes which will have knock-on benefits in other areas of your life including brain function, mental health, strength and reducing the risk of heart attack and stroke.
You could do 30 minutes of moderate exercise like walking, cycling or swimming 5 times a week. Or, if you prefer to spend less time, 15 minutes of vigorous activity like running, sports or fitness lessons 5 times a week. Walking to work, gardening or even carrying the shopping home can all add up and help you meet your activity goals12.
In terms of your diet, you can try to cut back on sugary drinks, salt, alcohol, red meat and processed food - especially when there's added sugar or salt. Choose to eat more wholegrains, vegetables and healthy fats like nuts, seeds and avocados. If you need a healthy sugar kick, apples, grapes and berries have been linked to lower risk of diabetes13.
Get tips on better health
Sign up to our emails on the better way to better health.
We'll keep you up-to-date with the latest research, expert articles and new ways to get more years of better health.


