
7 science-backed tips to optimise your HbA1c level and reduce diabetes risk
Key Takeaways
- Exercise, exercise, exercise
- Carbs - keep 'em complex
- Sleep 7-8 hours
- Don't eat just before bed
- Keep a low waist circumference
- Don’t smoke
- Reduce psychological stress
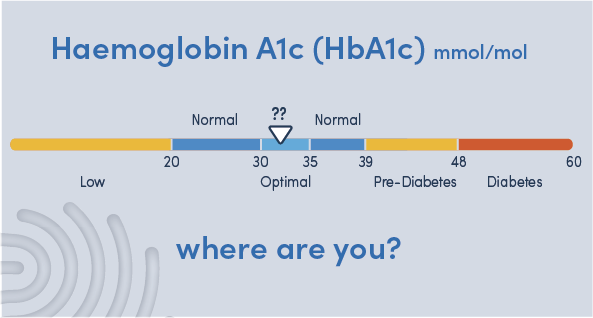
Haemoglobin A1c (HbA1c) measures how your body is handling your blood sugar and is a key marker of your metabolic health. At certain levels of HbA1c we say someone has “pre-diabetes” (high risk of developing diabetes) or “diabetes” but HbA1c is really on a continuum from good to poor sugar-handling.
But even before you get to diabetic levels, a higher HbA1c is associated with an increased risk of heart disease1 and cancer2.
So, if you don’t know your HbA1c, you should. Stop reading and order a Pre-diabetes & Sugar Handling HbA1c Test you can take at home.
Getting your HbA1c into the optimum range and keeping it there is one of the most important things you can do for your health. Our experts have scoured the latest science to bring you the top 7 things you can do to optimise your HbA1c and reduce your risk of diabetes.
1. Exercise, exercise, exercise…
Your muscles are metabolic powerhouses, burning through glucose and fat to keep your blood sugar levels in check. Exercise stimulates your muscles to pull glucose out of your blood and the effects last long after that last rep. Strength and aerobic training are probably the two most effective ways to optimise your HbA1c.
Gotta pump it up
You should aim for at least two strength (resistance) training sessions a week. Bigger, more metabolically active muscles handle blood sugar better. People who do regular resistance training are about 35% less likely to develop diabetes than people who don’t3. And it's never too late to start. Even in adults who already have type 2 diabetes, strength training has been shown to reduce HbA1c4. And the more they trained, the stronger they got and the more their HbA1c dropped.
Just do it
What’s better than strength training? Strength training combined with aerobic training! Moderate intensity “zone 2” training where your heart rate is about 60-70% of maximum for 45-90 minutes, 3-4 times a week is a staple for elite athletes and should be your go to. Remember, the intensity is relative to your fitness (60-70% of your maximum heart rate) so this is something we can all do.
Zone 2 training reprogrammes your metabolism, increasing the size and number of mitochondria in your muscles and burning harmful “visceral” fat (the fat around your organs which promotes insulin resistance and diabetes). As with strength training, studies confirm that regular aerobic exercise drops HbA1c as well as improving other metabolic health parameters like body weight and VO2 max5.

2. Carbs: keep 'em complex
After exercise, diet is the next big lever you can pull to optimise HbA1c. However, people respond to foods in different ways and food context - when you eat, how you slept, how much exercise you’re doing… - is at least as important as what you eat. That said, here are some general pointers backed by science:
Not all carbs are created equal
Refined carbohydrates have had fibre and other nutrients stripped out and are much easier for your body to digest than complex carbohydrate. Quick digestion and absorption leads to spikes in blood sugar, pushing up your HbA1c. Sugary drinks and fruit-juices in particular dump large amounts of sugar into your bloodstream and are best avoided unless you’re running marathons or doing the Tour de France.
A food’s “glycaemic index” tells you how quickly it will raise your blood sugar - a low GI index raises blood sugar slower than a high GI index6.
But it’s not all about the GI index. The amount of carbohydrate has a larger effect on blood sugar levels than the GI index. A recent randomised controlled trial showed that lowering carb intake to 40-60g per day lowered HbA1c compared to a standard diet7. Taking this to the extreme and virtually eliminating carbohydrate from your diet - called a ketogenic diet - has also been shown to improve HbA1c8.

Get your fibre fix
Fruits, vegetables and nuts contain plenty of fibre which you can’t absorb, helping you feel full without boosting your sugar levels. Fibre also feeds your gut microbiome so it’s great for your gut health too. Lastly, fruit and veg contain active compounds, such as polyphenols and glucosinolates, which can lower your HbA1c. This explains why studies show that a higher intake of fruit and vegetables is associated with a lower risk of diabetes9.
3. Sleep tight
Sleep is the unsung hero of metabolic health. Data shows that sleeping less than 5 hours or more than 8 hours a night is associated with a higher HbA1c level10. Why does this happen? If you don’t get enough sleep your body becomes insulin resistant and less able to control blood sugar quickly.
One study took 7 young, healthy volunteers and showed that just 4 nights of sleeping less than 5 hours was enough to cause profound insulin resistance11.

Getting 7-8 hours of good quality sleep a night is as important as exercising and eating well.
4. When you eat matters
You probably know that your body has a 24 cycle called your circadian rhythm. Did you also know that this affects how you metabolise food?
Studies have shown that eating more of your calories earlier in the day improves fasting sugar levels12.
In particular, it’s best to avoid eating your last meal close (within 2-3hrs) to when you go to bed as this not only worsens the quality of your sleep13 but is also associated with a higher HbA1c14.
5. Your waist doesn't lie
We talk about weight a lot but actually studies suggest that waist circumference (WC) or waist to hip ratio (WHR) is a better indicator of metabolic health than body mass index (BMI). WHR correlates better with the amount visceral fat in your body15 and has a stronger, more consistent association with overall mortality16.
Higher WC is associated with higher HbA1c17 and can predict who will go onto develop diabetes18.
Based on the evidence, men should keep their waist circumference under 90cm and women should aim for less than 80cm19.

6. Kick the habit
We all know that smoking is bad for us, but did you know that smoking is a direct cause of diabetes? HbA1c levels are highest in smokers and lowest in non-smokers, with ex-smokers somewhere in the middle20. Smokers are 30-40% more likely to develop diabetes than non-smokers21.
7. Take a chill pill
Stress can impact all areas of your life, including your HbA1c levels. Psychological stress causes your body to release adrenaline and cortisol which increase your blood sugar. High job stress is correlated with a higher HbA1c22, 23 and major stressful life events are associated with the onset of diabetes24.
On the plus side, a recent randomised trial showed that stress-reduction techniques could reduce HbA1c25.
Are there areas in your life that could benefit from reduced stress? Mindful practices like meditation and gratitude journaling can help you to take back control and feel more grounded.

What if I need support?
Good sugar-handling is crucial to good health and we should all aim to have our HbA1c in the optimal range.
But we know it’s not easy to do all of the above tips alone, so that’s why you don’t have to. Selph can help you get there with our 12-week Health Reset Programme. Our health coaches can support you to reach your health goals and give you tools you can rely on time and again after finishing the programme and beyond. We’ll help you become the master of your health.
Take the first step towards your best health today and book a free discovery call to start your journey.
We're on a journey to becoming the first longevity company and we'd love to bring you along.
Sign up to get our twice monthly Selph Improvement newsletter which is packed with evidence-based tips to optimise your health.
We'll also keep you up-to-date with articles, products and services that are all designed to turn the latest science into more years of better health for you.
